Blog: The Future for National Clinical Audit
Published: 07 Feb 2022
By HQIP’s Medical Director Danny Keenan
I wanted to give you an update on development in the National Clinical Audit and Patients Outcome Programme (NCAPOP). As we approach a new year, I thought that it would be worth you seeing the direction that we wish to take the programme during 2022 and beyond.
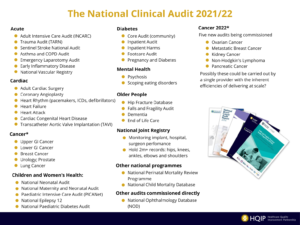
All of you are likely to touch on some aspect or other of the programme. The Appendix includes the topics covered.
During the early days of the pandemic, we took a critical look at the programme and considered if it was still fit for purpose and was it ready to move into the truly digital era that is bound to be with us when we finally leave the pandemic behind.
The review took the place of a series of in-house discussions and, importantly, a series of two-hour webinars conducted with interested methodologists, audit providers, clinicians (who could be spared) and HQIP staff. We had a specific webinar which included HQIP’s service user group where we considered the patient perspective.
The conclusions were:
The programme is regarded as very valuable by the service, clinicians and users, but there are things that need to change to make it more effective at supporting improvement in patient outcomes.
The drawbacks:
- Audits have many metrics and some include research elements beyond reviews against standards.
- There is burden to the service in participation and this must be matched by the utility of output back to the service. Key findings can be obscured by reporting back in large, hard to read, annual reports
- Timeliness – the ideal is real time data to drive local quality improvement (QI).
- Moving beyond mortality outcomes to include meaningful patient outcomes
We are looking to address these by:
Burden
Reducing the number of metrics down to ten and if there is a requirement for more than this, then this needs justification.
Ensuring that routine data is used if at all possible (currently 67% of input is routine). This requires linkage with NHS Digital to ensure the smooth flow of such data and linking with electronic patient records in the future.
Outputs
A move to slim down the annual report so that it is a much tighter document, more easily readable and focused on a major finding from the latest review, with corresponding websites used to display more in-depth findings and data.
Getting the outputs back to as many different partners as possible is really important. There are multiple audiences including patients and the public (including the media), the service, commissioners, clinicians and researchers. The methods of addressing each of these groups can be different and needs addressing. We have used several approaches:
- We have worked with the informatics team at the CQC to produce single page pdfs of the latest results, concentrating on the key metrics. This has been well liked by the service with multiple hits on our website.
- Similar results are going to be displayed on the Model Health System with Emergency Laparotomy already available and five more audits to follow. Again, this is directed at the service.
- The audit providers are now producing infographics displaying, on a single page, the key findings which all find easy to follow.
- We work with NHSEI presenting the latest reports bimonthly at a meeting reporting to the National Quality Board so that none of the national recommendations go unheeded.
- In addition, however, each of the audit providers and their associated clinical groups present their results in multiple additional media, which should ensure dissemination in the clinical community.
Timeliness
A further output from the review was the need to get data back to the service as quickly as possible. This was hotly debated as faster data is likely less assured. We have reached a solution with getting fast data back while still having the assurance of the yearly data. As we commission and re-commission, we are specifying that whilst there should be an annual report focusing on the main message of the year, there should be three-monthly online data outputs directly to the service for quick quality improvement activity. We hope that as we use quick data more, the assurance will follow it.
Patient Outcomes
Our review highlighted that we needed to do more to introduce more patient reported outcomes. There are very important outcomes included such as mortality, post-operative sepsis and readmission, but there is a gap and we intend to help audit providers bridge this as we re-commission audits within NCAPOP.
All of this, however, it still begs the question as to whether the programme is making a difference for patients. We believe it is because the programme exists to provide all with assurance that our services are performing to the standards set and as a very important stimulus for local quality improvement.
Here is a screen shot of the output from the Hip Fracture Database showing the six key metrics benchmarked across England. One can see how this particular Trust is performing. As with all these NCAB displays, virtually all Trusts will have an area where they can do better. By displaying such results (and these are all openly reported results with no passwords), colleagues at all levels can focus on a Quality Improvement initiative from such results.

The programme is very closely aligned to NICE standards, and where there are none, to College or other evidenced based guidance. We audit against such standards and by seeking out variance, shine a light so that the service and others can act to rectify such variation. We work closely with GIRFT who call on the results as they review different services so that there is this additional impetus to improve. In addition, by such alignment, there will only be “one version of the truth” so that the service does not receive conflicting messages.
I hope this has given you a taste of what the programme is achieving and hopes to achieve in the next few years. We would like to extend our thanks to all in the clinical community, and their leaders, who by their selfless actions have helped keep the NCAPOP to the fore in its assurance and improvement of our clinical services. I would be more than happy to discuss any aspects of this further, depending on the interests of members.

Danny Keenan
HQIP Medical Director
The Appendix